Two Sides of the ‘Cancer Coin’
Cancer prevention and cancer survivorship represent two sides of the ‘cancer coin’; both represent strategies to deal with cancer either after cancer treatment (survivorship) or before cancer arises (prevention).
According to the Canadian Cancer Society, it is estimated that 7500 Canadians were diagnosed with head and neck cancers in 2022. Head and neck cancers are malignant tumours found in the mouth, nose or throat, larynx, lips or salivary glands. Many individuals are unaware of the danger or even existence of head and neck cancers.
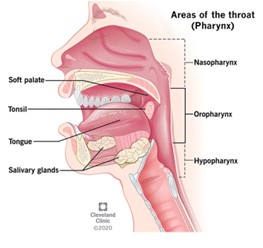
Well established causes of head and neck cancers are smoking and consumption of large quantities of alcohol. What many people don’t know is that the HPV virus is also associated with head and neck cancers. Although largely associated with unprotected sex, infection with the human papillomavirus (HPV) can also increase the risk of head and neck cancers. Indeed, HPV-related oropharyngeal (the middle part of the throat behind the mouth) cancers are on the rise in Canada.
Although these types of cancers are aggressive, the risk of developing a head and neck cancer is largely preventable with the practice of healthy lifestyles and HPV immunization. The incidence of non-HPV oropharyngeal cancer is decreasing in developed countries, possibly due to declining levels of smoking. However, HPV-related oropharyngeal cancers are on the rise in these countries, contributing to an epidemic of virus‐induced cancers.
Prevention
Vaccination against HPV-associated cancers is highly effective. In Canada, HPV vaccines are provided under publicly funded programs to individuals 18 years or younger and those who are at increased risk. The current vaccine uptake rates in Canada varies. In addition, lifestyle changes are also needed to fight the head and neck cancer burden. Dr. Violet D’Souza, an Assistant Professor in the Faculty of Dentistry, and Associate member of the Beatrice Hunter Cancer Research Institute, is interested in creating head and neck cancer awareness among Dalhousie University students.
Dr. D’Souza and Jacob Pete, a 3rd year dental student recently conducted an anonymous survey with Dalhousie students to explore students’ knowledge about head and neck cancers and their willingness to receive HPV vaccines to prevent HPV-related head and neck cancers. While most respondents had heard about head and neck cancers, only about one-third knew these cancers are preventable. When asked what may cause these cancers, the vast majority sited tobacco use and alcohol consumption, however less than half sited viral infections.
“HPV vaccine uptake is crucial. We must work together to achieve it,” says Dr. D’Souza.
Increasing insights into how head and neck cancers arise are contributing to better cancer-prevention strategies. Nevertheless, cancers will continue to occur at some level and there must be increased attention paid to how best to improve the quality of life for those who have undergone head and neck cancer treatment.
Survivorship
Recent advancements have led to a net survival of at least five years, for people with head and neck cancers. Head and neck cancers can have an impact beyond the diagnosis, affecting overall well-being in terms of nutrition intake, frailty, a dependency on caregivers and increases healthcare utilization posing a significant economic burden. Identifying gaps in planning a targeted, person-centred survivorship roadmap for survivors is essential. Cancer survivors frequently encounter significant medical, financial, psychosocial, and functional challenges. As a dental public health specialist, Dr. D’Souza is a passionate advocate for head and neck cancer survivors, the challenges they face, and how these challenges lead to oral health deficits and affects a patient’s overall well-being in terms of nutrition intake, frailty, and dependency on caregivers. “Head and neck cancer survivorship care should include timely assessment of oral health and functions,” explains Dr. D’Souza.
“Healthcare professionals, including doctors, dentists, dental hygienists, and nurses, should proactively educate their patients, identify at-risk people, and direct them to appropriate resources.”
