A multi-pronged approach to myeloma research
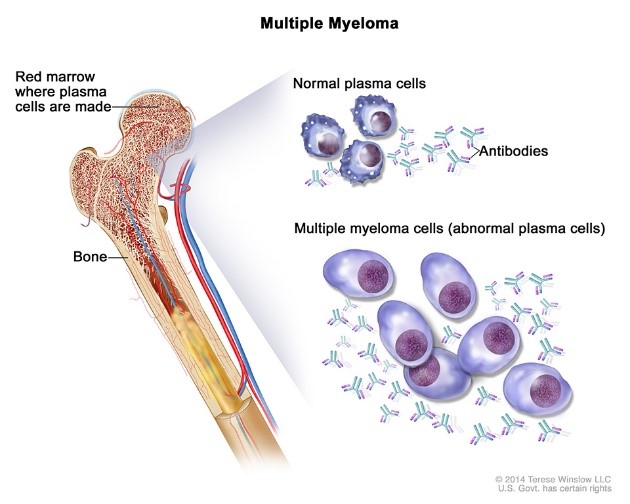
Myeloma, or multiple myeloma is a cancer that starts in white blood cells (plasma cells). These cells are mainly found in bone marrow. When plasma cells change or no longer behave normally, myeloma can occur.
Stock Image
Multiple myeloma is when there are many of these abnormal plasma cells in the bone marrow, making it difficult for other blood cells to work normally.

Anthony Reiman
BHCRI Senior Scientist Dr. Anthony Reiman is a medical oncologist at Horizon Health in Saint John, New Brunswick, with academic appointments at both Dalhousie and University of New Brunswick. He has been seeing cancer patients for over twenty years, including many with multiple myeloma. As a researcher conducting clinical trials, Dr. Reiman can bring new, innovative treatments to his patients, often many years before these new treatments might otherwise be available. Clinical trials also help answer important questions about the best way to use new treatments and generate evidence that organizations like Health Canada and the Canadian Agency for Drugs and Technologies in Health (CADTH) need to determine whether these new treatments should be provided as a new standard of care. “We have been pleased to introduce new therapies through trials and have contributed to trials that have changed the way we treat myeloma in Canada and around the world”, says Dr. Reiman.
Multiple myeloma is seen more commonly in people as they age, in men more than women and in people of African decent more than Caucasian. The good news is that the life expectancy is now approaching 10 years instead of three years as has been the case for these patients. Even for frail and elderly patients who cannot be treated intensively, the average lifespan has increased to about five years. This is a substantial improvement in the last 20 years since there are twice as many myeloma cases diagnosed in Canada every year compared to twenty years ago.
As the population ages, more people are being diagnosed with cancer and with myeloma in particular. “But even when you account for the aging of our population and the increasing size of our population, the rate at which people are diagnosed with myeloma almost still seems to be increasing,” “and we don’t know why that is.”
Gaining essential new knowledge to improve cancer treatment demands access to patient samples. Samples from cancer patients allow detailed study to determine how a cancer is behaving and what treatments may be effective. Access to such patient samples requires a specialized facility termed a biobank. Dr. Reiman and other researchers in the region now have access to well organized and managed biobanks.

Manal Elnenaei
The Atlantic region is home to two myeloma tumour banks; one in Dr. Reiman’s laboratory at Dalhousie Medicine New Brunswick and the second at the QEII Health Sciences Centre in Halifax, led by BHCRI member Dr. Manal Elnenaei. The team is supported by the installation of sophisticated machines which can determine changes in a tumour’s genetic makeup. These essential machines (that perform what is termed next generation sequencing) were purchased through a generous donation with the proviso that myeloma research would comprise some of the utility of these machines. Cancer researchers in the region can acquire patient samples housed within the biobank to allow fundamental and clinical research on multiple myeloma.
These tumour banks also facilitate collaboration among clinical scientists and basic scientists to further advance multiple myeloma research.


Mahboubeh Rahmani Shashi Gujar
BHCRI members Dr. Mahboubeh Rahmani and Dr. Shashi Gujar are collaborating to utilize specimens from the tumour bank, to explore how changes in metabolism of myeloma cells might impact the ability of some treatments for multiple myeloma. The team of researchers dedicated to finding better treatments for multiple myeloma bring different expertise and approaches to a common goal. These combined efforts on multiple myeloma research are aimed at understanding the underlying factors that lead to this incurable cancer. The team is committed both to improve the effectiveness of existing treatments and to pave the way for innovative new precision therapies.
Patients are now also becoming active participants in research, getting involved from the very beginning. Patients are driving the questions that researchers now ask and becoming integral members of the research team. Working with groups like Myeloma Canada, researchers can connect with myeloma patients and their support network, to help identify research priorities.
Even though myeloma largely remains an incurable cancer, recent advances give realistic hope to one day find a cure or to continue to further extend a patients life expectancy and their quality of life. Advances in myeloma treatment have come with the harnessing of the immune system to fight cancer. There are several promising immune therapy approaches that are currently in clinical trails, including trials in Halifax. One of these new approaches is CAR (Chimeric Antigen Receptor) -T cell therapy. CAR-T uses a patients’ own cells, which are modified to help fight the cancer. For clinician researchers like Dr. Reiman, “Being able to conduct leading edge research in the region is important for patients and clinicians – being part of the solution and bringing advances to our patients as soon as we can.”
